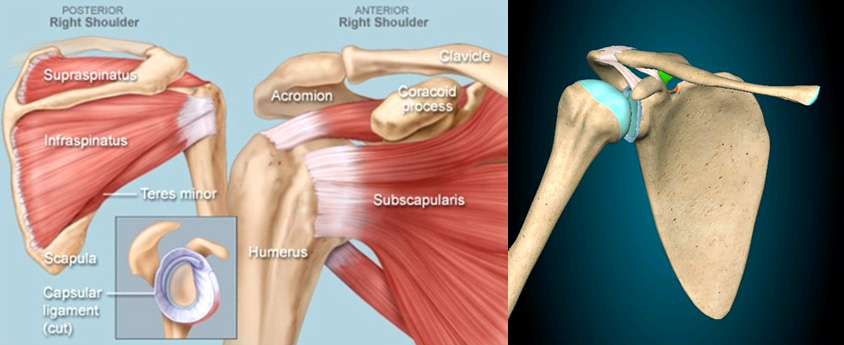
The shoulder is a “ball-and-socket” joint made up of the upper arm bone (humerus), shoulder blade (scapula) and collarbone (clavicle).
This increased range of motion of shoulder joint comes at the compromise of the stability of joint, making it more prone to injury and instability.
The majority of these conditions are effectively managed without surgical intervention; the surgical intervention is warranted in few conditions for thorough correction of the condition and allowing the patients to maintain an active and healthy life.
In order to determine the cause of your pain, your doctor will ask for details about your symptoms and medical history, and also perform a physical examination to evaluate the shoulder.
While X-rays are the basic investigations in Shoulder Orthopaedics to examine the bone architecture, alignment, fractures, Arthritis of the joint or calcium deposits in the soft tissues (tendons), MRI scans may also be performed in order to examine the bones and soft tissues of the shoulder.
Shoulder Arthroscopy is a minimally invasive procedure which is gold standard in diagnosis and treatment of several pathologies with the help of fibre-optic device and the internal image is projected on the screen. With the help of tiny surgical instruments into small incisions the procedure is performed. During the procedure the arthroscope is inserted through small incisions into the joint. The internal anatomy image is processed and projected onto the monitor or screen. The surgeon examines all the tissues in the joint from 1 to 3 small incisions. The viable tissue optimum for healing are repaired, the inflamed and damaged tissues are removed and loose bone fragments are excised in the procedure.

Patients can benefit from less tissue-damage, less pain, shorter recovery times and less scarring with arthroscopic techniques. Shoulder arthroscopy can be used to treat rotator cuff tears, labral tears, impingement, biceps tendonitis and AC joint arthritis. The type of repair performed depends on each patient’s individual condition, but often involves removing inflamed tissue, reattaching torn tissue or replacing damaged cartilage.
The clavicle, commonly known as the collarbone, is the bone of the shoulder joint that connects the arm to the trunk. Clavicle fractures most frequently occur as a result of trauma from a blow to the shoulder, fall or motor vehicle accident. They are most common in young children and older adults who are more susceptible to fractures.
The Clavicle is an important connection between the extremities and truck that also play a vital role in weight transmission from the extremities to the rest of the body. Clavicle fractures cause the shoulder to slump downward and a bruise to appear over the fractured area.
Pain is often experienced at the time of fracture and when the area is touched. Patients may also experience pain while trying to move the arm.
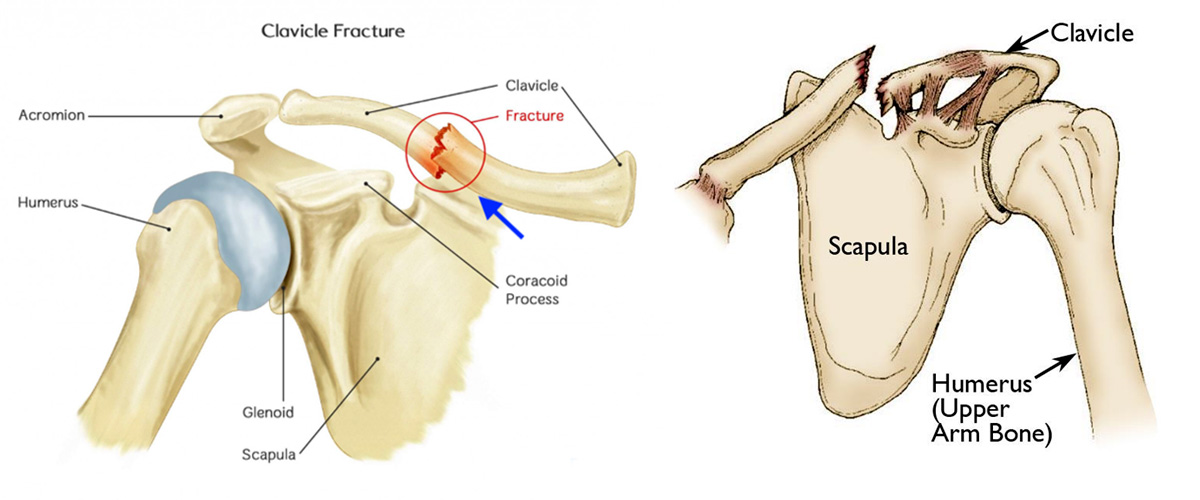
Many fractured collarbones can be treated through conservative methods such as immobilization, NSAIDS, and a sling. Clavicle fractures will most often heal on their own, with little intervention, but there are fractures that are best treated surgically and therefore the need to have the fracture evaluated. You may be instructed to wear a sling until pain subsides, which can take two to six weeks depending on your age and the severity of your fracture.
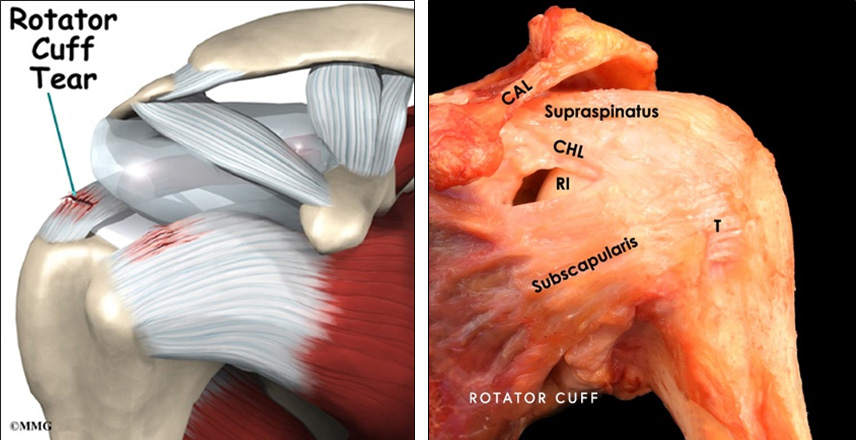
The rotator cuff is a group of tendons and muscles that support the shoulder joint and allow for complete movement while keeping the ball of the arm bone in the shoulder socket.
These tendons and muscles may become torn or otherwise damaged from injury or overuse (degenerative) and or trauma leading to pain, weakness and inflammation.
The tears that are well compensated can be treated without surgery. The Cuff lesions that are managed conservatively, needs a close follow up as there is a risk of progression of the tears.
The tear progression corresponds to retraction of the tendon and Fatty infiltration of the muscle belly.
The surgery is indicated in any patient with
The Surgery is typically indicated to repair complete tears with loss of function. The surgery is mainly performed for the loss of function than the relief from pain. 15 % patients still continue to have persistent pain after surgery.
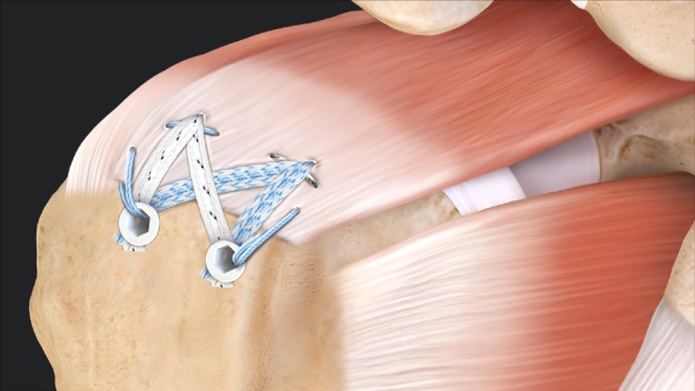
Rotator cuff surgery is now performed arthroscopically rather than through an open procedure even for the most severe tears. The procedure involves reattaching the torn tendon back to the bone and is typically performed setting under general anaesthesia. The Rotator torn tendons are attached to the bone with the help of bio-absorbable anchors that have fibre tapes (non-absorbable sutures) attached to it.
The repairs performed over massive tears (>5cm retraction or 2 or more tendon involvement may have difficult healing of tendon to bone. In patients with grade > 2 fatty infiltration cuff surgery is differed and patient may have to one of the undergo salvage procedures. The Reverse Shoulder Arthroplasty may be indicated in irreparable cuff tears with cuff arthropathy patients. The outcome of the surgery may also deteriorate with smoking, age (after 63 – 65 years), inferior tissue quality and osteoporosis.
The labrum is a protective ring of cartilage around the glenoid socket that provides stability, cushioning as well as an attachment for the stabilizing ligaments of the shoulder joint
A tear in the labrum is caused by injury (dislocation of the shoulder joint) or overuse and can lead to pain and “catching” of the joint. While many labral tears can be treated by managing pain symptoms and undergoing protective strengthening in physical therapy, many tears depending on location require surgical treatment.
The Labral repair surgery is now performed arthroscopically rather than through an open procedure even for the most severe tears. The procedure involves reattaching the torn labrum back to the bone with the help of suture anchors and is typically performed under general anaesthesia.
The back to sport activity time is typically 4 to 6 months after surgery.
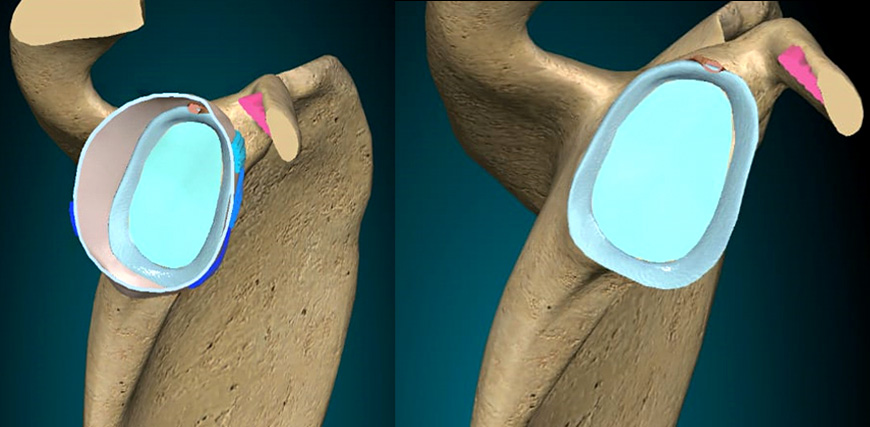
The shoulder is a “ball-and-socket” joint where the “ball” is the rounded top of the arm bone (humerus) and the “socket” is the cup (glenoid) of the shoulder blade.
A layer of cartilage called the labrum cushions and deepens the socket.
A dislocation occurs when the humerus completely pops out of its socket, and a subluxation occurs when there is a partial or incomplete dislocation.
As the body’s most mobile joint, able to move in many directions, the shoulder is most vulnerable to dislocation.
Dislocation causes pain and unsteadiness in the shoulder. Other symptoms may include swelling, numbness, weakness and bruising.
The majority of dislocations occur when the humerus slips forward, a condition called anterior instability. The humerus is also capable of dislocating backwards or downwards. In most cases, the dislocated shoulder can be manipulated back into place by a doctor in a process known as closed reduction.
While most dislocations occur from trauma, partial dislocations or subluxations often occur from overuse injuries during overhead activities. Throwing sports, volleyball, weight lifting and other overhead sports will commonly lead to subluxation events and symptoms.
The shoulder dislocations and subluxations can lead to a labrum or cartilage tear, tendon or ligament injuries, and blood vessel and nerve damage. Shoulders that have dislocated once are more likely to dislocate in the future, potentially resulting in further shoulder instability, weakness, and damage.
Shoulder surgical stabilization can be performed through an arthroscopic procedure that involves reattaching loose or torn ligaments (labrum and capsule) to the joint socket (glenoid) with the use of special implants called suture anchors. These anchors have sutures attached that are used to repair and tighten the torn ligaments. The newer anchors will be absorbed over time or are made of a larger suture material that avoids implanting metal.
Depending on the associated injuries from the instability, additional surgery may be required involving tightening of the shoulder capsule (lining) and repair tears of the rotator cuff.
The Patients with glenoid bone loss may need a mini open surgery depending upon the bone loss from socket side and ball side.
One of the most common causes of shoulder pain, impingement occurs when the front of the shoulder blade bone, call the acromion, rubs against the rotator cuff as a person lifts his/her arm. The rotator cuff is a group of muscles and tendons that stabilizes the shoulder and permits lifting and rotating movements. If the rotator cuff weakens or is injured, the bone of the upper arm (humerus) can lift up, pinching the rotator cuff against the acromion. The muscles can then swell further, creating a vicious cycle of pain and weakness that will not improve without intervention.
In addition to rotator cuff injuries such as tendonitis and tearing, impingement may be the result of bursitis, an inflammation of the bursa cushioning sac between the rotator cuff and the acromion.
Impingement worsens over time. At first, you may feel mild pain in the shoulder, which may radiate from the front of the shoulder to the side of the arm. The pain may worsen when you lift your arm, reach for something, or throw or serve a ball while playing a sport. There may be some swelling and tenderness at the front of the shoulder as well. As impingement progresses, pain and stiffness worsen until you may not be able to lift or lower your arm without extreme pain.
People most at risk for developing impingement are athletes, especially those who swim or play baseball or tennis, and people whose occupations include repetitive lifting or overhead movements, such as painting and construction. Sometimes, impingement occurs after a minor injury, or just from performing activities of daily living.
Frozen shoulder, also known as adhesive capsulitis, is a common condition that causes pain and stiffness in the shoulder as a result of a tightening or thickening of the capsule that protects the structures of the shoulder. Although the specific cause of this condition is not known, it most often occurs after recent immobilization of the joint or as a complication of diabetes. Frozen shoulder most often affects patients between the ages of 40 and 60.
Patients with frozen shoulder often experience pain, stiffness and limited range of motion that gradually worsens as the joint becomes more and more frozen. Eventually, the shoulder will shift into its thawing phase, during which pain and stiffness subside and range of motion is slowly restored.
Your doctor can diagnose frozen shoulder after a thorough evaluation of your condition, as well as an X-ray or MRI examination, which helps rule out other possible shoulder conditions.
Treatment for frozen shoulder usually focuses on managing pain and other symptoms as the condition progresses. This may include anti-inflammatory medications, corticosteroids and physical therapy. Minimally invasive surgical procedures, such as arthroscopy and manipulation, may also be performed with a goal of stretching or releasing the contracted joint capsule.
Dr. Omkar is excellent Doctor. My 11 year old son fallen down while playing with both fracture wrist. Left hand wrist operation was so critical and 2-3 Doctors refused to do this operation but Dr. Omkar has given us hope and started the operation immediately after admitted my son at the SRV Hospital-Chembur. His study, observation and experience is too good. He is also a very helpful person as human being.
Dr. Omkar Sadigale is very knowledgeable. He diagnosed my wife’s ankle fracture correctly which other doctors could not do. He follows full ethical practices so you are assured that you are in safe hands. I would highly recommend Dr. Omkar Sadigale for any orthopedic or bone surgery related needs.
Best doctor I ever came across! SRV hospital rocks only because they have Dr. Omkar in their hospital as the best orthopedic!! Excellent guidance throughout and for any issues just a call away be it whatever time day or time blessed to have such Dr's whom we trust with our treatments and they don't let us down!
I had a toe fracture as I fell while parking my two wheeler. I was immediately taken to SRV hospital, Chembur under the care and treatment of doctor Omkar Sadigale. Thereafter everything was well handled and taken care by dr.Omkar. There was a small operation conducted on my toe to realign the fractured bones. Now I am fine and able to walk. He is one of the best orthopaedic in Mumbai.
My son has got hip and shoulder fractures due to conversion. I admitted him to SRV Chembur due to RTPCR positive. To be great humanity Dr. Omkar was there at that time in hospital. When I met him at that time I had confidence that I am at the right place. He checked my son and carried operation on the same day afternoon. during the operation, he boosts my morale...Read More